The Complete Guide to Health Checks: Why Regular Screenings Save Lives and Reduce Healthcare Costs
A health check is far more than a routine doctor’s visit—it is a proactive, systematic assessment of your physical well-being designed to identify potential health risks before they become serious conditions. In an era where chronic disease accounts for 71% of all deaths globally, annual comprehensive health checks have become an indispensable pillar of modern preventive healthcare. Clinical research demonstrates that individuals who undergo regular preventive health assessments experience a 45% reduction in all-cause mortality risk, significantly lower rates of chronic disease-related complications, and dramatically reduced long-term healthcare costs. This article explores the science of health checks, their essential components, gender and age-specific screening recommendations, real-world case studies, and the rapidly expanding global market driving investment in preventive health services.
What Is a Health Check and Why Does It Matter?
A comprehensive health check involves multiple diagnostic tests, physical examinations, and health assessments performed on asymptomatic individuals to achieve three primary goals: (1) early detection of disease when treatment is most effective, (2) identification of risk factors that enable preventive intervention, and (3) behavioral counseling to support lifestyle modifications that reduce future disease risk.
The transformative power of health checks lies in early detection. Research shows that women undergoing regular mammography screening have a 40% lower likelihood of dying from breast cancer compared to those who do not participate in screenings. Similarly, early-stage lung cancer diagnosis dramatically improves survival rates, and early detection of prostate cancer prevents serious complications and enables better treatment outcomes. Globally, studies estimate that approximately 40% of cancer-related deaths, 80% of type 2 diabetes deaths, and 80% of cardiovascular disease deaths could be prevented through routine annual health screenings and timely intervention.
Beyond mortality reduction, health checks deliver profound economic benefits. By identifying conditions in asymptomatic stages, they allow for lifestyle modifications, dietary changes, and targeted medical interventions that prevent disease progression and the need for expensive advanced treatments. The cost-effectiveness is substantial: investing in a comprehensive health check ($200–500 depending on location and depth) can prevent the need for $10,000–50,000+ in advanced disease management, hospitalization, and chronic disease care.
Core Components of a Comprehensive Health Check
A baseline health check typically includes the following standardized assessments:
Physical Assessment
- Vital signs monitoring: Blood pressure, heart rate, respiratory rate, body temperature, and oxygen saturation (SpO₂)
- Anthropometric measurements: Height, weight, and body mass index (BMI) calculation
- Physical examination: General assessment of skin, eyes, ears, nose, throat (ENT), cardiovascular auscultation, respiratory assessment, abdominal palpation, and neurological screening
Laboratory Tests
- Complete blood count (CBC): Detects anemia, infection, and blood cell disorders
- Lipid panel: Measures total cholesterol, LDL, HDL, and triglycerides to assess cardiovascular risk
- Fasting blood glucose or HbA1C: Screens for prediabetes and type 2 diabetes
- Liver function tests (LFTs): Assesses hepatic health; ALT, AST, bilirubin, alkaline phosphatase
- Kidney function tests (KFTs): Measures creatinine, blood urea nitrogen (BUN), and eGFR; identifies renal disease
- Thyroid function (TSH, Free T3, Free T4): Screens for hypo- and hyperthyroidism
- Urinalysis: Detects infections, glucose, protein, and kidney dysfunction
Diagnostic Imaging (Age and Risk Dependent)
- ECG (Electrocardiogram): Screens for arrhythmias, ischemia, and structural heart disease
- Chest X-ray: Baseline imaging for lung, cardiac, and mediastinal assessment
- Ultrasound: Abdominal imaging to assess liver, gallbladder, pancreas, spleen, and kidneys
Gender-Specific Screenings
These are tailored based on biological and epidemiological risk factors, discussed below.
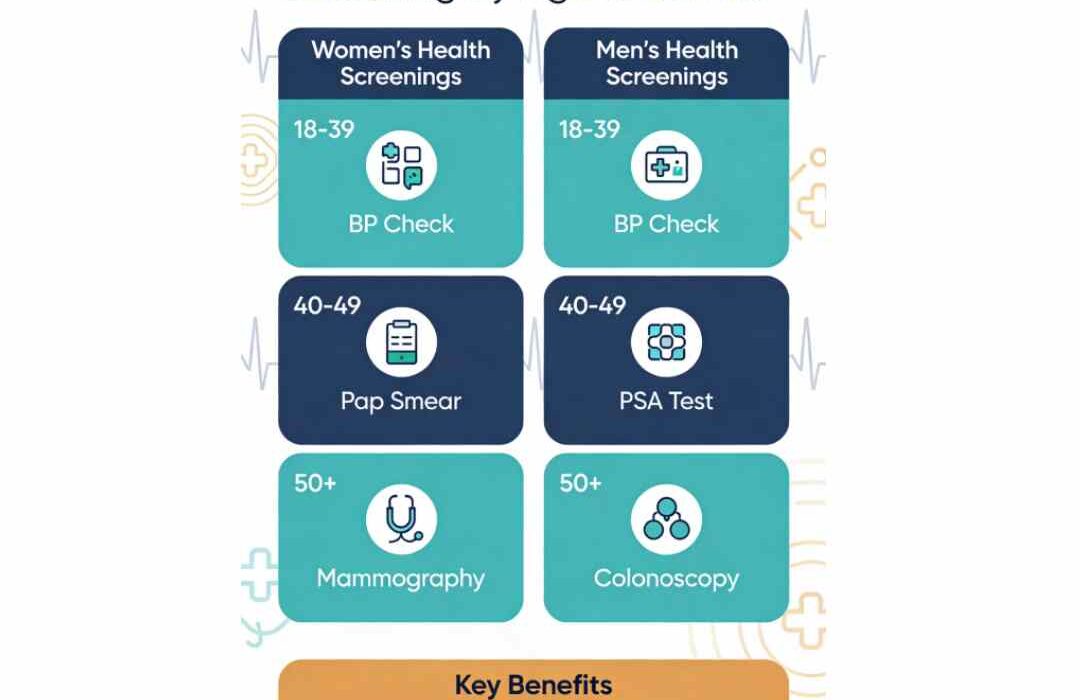
Age and Gender-Specific Health Screening Recommendations
Health screening recommendations vary significantly by age and gender, reflecting different epidemiological risks and the optimal timing for early disease detection.
Screening Guidelines for Women
| Age Group | Key Screenings | Frequency | Clinical Significance |
| 18–39 years | Blood pressure, cholesterol, STI screening, Pap smear (if sexually active, age 21+), clinical breast exam | Baseline BP/lipids; Pap every 3 years (age 21+) | Early detection of cervical dysplasia; baseline cardiovascular risk assessment |
| 40–49 years | Mammogram (baseline or per risk), blood pressure, cholesterol, pelvic exam, bone density assessment (if risk factors) | BP/lipids every 1–2 years; mammogram annually or every 1–2 years depending on risk | Breast cancer early detection; assess menopause-related risks |
| 50+ years | Mammogram, pap smear (until age 65), blood pressure, lipids, bone density (DEXA scan), colorectal cancer screening, diabetes screening | Annual or per physician recommendation | Osteoporosis risk escalates post-menopause; colorectal cancer risk increases; continued breast cancer surveillance |
Why Gender Matters: Women face elevated risks for breast cancer, cervical cancer, osteoporosis (especially post-menopause), and autoimmune conditions. Early mammography and Pap screening have proven to reduce mortality from these conditions by 40–43%.
Screening Guidelines for Men
| Age Group | Key Screenings | Frequency | Clinical Significance |
| 18–39 years | Blood pressure, cholesterol, STI screening (sexually active), mental health screening, diet/exercise counseling | Baseline BP/lipids; STI screening per risk | Establish cardiovascular baseline; address lifestyle risk factors |
| 40–49 years | Blood pressure (annually), cholesterol (every 4–6 years), prostate cancer discussion (PSA per risk/preference), diabetes screening | BP annually; lipids every 4–6 years; PSA per discussion | Cardiovascular disease risk escalates; prostate cancer awareness initiated |
| 50+ years | Blood pressure, cholesterol, colorectal cancer screening (colonoscopy every 10 years, age 45 onward), prostate screening (PSA per individual risk), diabetes screening, lung cancer screening (if smoking history) | Annual BP; colonoscopy/FOBT as recommended; PSA/DRE per risk | Colorectal cancer risk increases; prostate cancer peak incidence; smoking-related disease surveillance |
Why Gender Matters: Men generally develop cardiovascular disease earlier than women and have higher rates of prostate and colorectal cancers. Prostate cancer screening remains controversial but should be discussed individually based on age, family history, and personal risk tolerance.
Case Study 1: Early Breast Cancer Detection in a 48-Year-Old Female
Patient Profile
A 48-year-old woman, nonsmoker, no significant past medical history, and no family history of breast cancer, presented for routine annual health screening. She reported no breast symptoms or concerns. Physical examination by her physician was normal.
Intervention
As per age-appropriate screening guidelines, a mammogram was ordered. The imaging revealed a 0.8 cm nodular density in the upper outer quadrant of the left breast—not palpable clinically but identified through mammographic screening.
Diagnostic Follow-Up and Case Outcomes
- Year 1 (2024): Mammography detected lesion → referred to breast surgeon → ultrasound and biopsy performed → pathology confirmed invasive ductal carcinoma (IDC), grade 2, hormone receptor positive
- Year 2 (2025): Surgical lumpectomy performed; margins negative; sentinel lymph node biopsy negative (Stage I cancer)
- Year 3 (2026): Adjuvant radiation therapy + endocrine therapy initiated; regular mammographic surveillance continues
Critical Outcome Analysis
By age: 48, this patient’s cancer was detected at Stage I (localized disease) due to routine mammographic screening. At this stage, five-year survival rate exceeds 99%. Had screening been delayed by 3–5 years and the cancer progressed to Stage III or IV, five-year survival would drop to 70% or lower. The early detection prevented the need for chemotherapy (a Stage III protocol), reduced treatment burden, and enabled breast-conserving surgery rather than mastectomy. Estimated healthcare cost savings from early detection: USD 50,000–100,000+ in avoided advanced cancer treatment.
This case exemplifies why routine mammography is a life-saving intervention for women age 40+, particularly those with family history or other risk factors.
Case Study 2: Prediabetes Detection and Prevention in a 52-Year-Old Male
Patient Profile
A 52-year-old male executive presented for annual health check. Overweight (BMI 28.5), sedentary lifestyle (desk job), no diabetes history, but father had type 2 diabetes diagnosed at age 58. No current symptoms of diabetes.
Intervention
Annual health screening included fasting blood glucose and HbA1C. Results: Fasting glucose 118 mg/dL (normal < 100) and HbA1C 5.9% (prediabetic range 5.7–6.4%). Blood pressure elevated at 138/86 mmHg. Lipid panel showed elevated triglycerides (198 mg/dL) and low HDL (38 mg/dL)—metabolic syndrome indicators.
Outcomes Across Three Years
- Year 1 (2024): Prediabetes and metabolic syndrome diagnosed via routine screening. Patient referred to lifestyle intervention program: dietary counseling (reduced refined carbohydrates, increased fiber), structured exercise program (150 min/week moderate activity), weight loss goal of 5–10%.
- Year 2 (2025): Repeat HbA1C 5.5% (improved); weight reduced by 6 kg; blood pressure normalized to 128/78 mmHg; lipids improved (triglycerides 165 mg/dL, HDL 42 mg/dL). Lifestyle modifications sustained.
- Year 3 (2026): HbA1C 5.4% (normal); maintained weight loss; BP stable; lipid profile normal. Type 2 diabetes development prevented through early intervention.
Cost-Benefit Analysis
Without early detection, this patient would have likely progressed to overt type 2 diabetes within 3–5 years, requiring pharmaceutical treatment (metformin, GLP-1 agonists), intensified monitoring, and significantly increased lifetime healthcare expenditures. Early detection enabled preventive lifestyle intervention, avoiding:
- Pharmaceutical costs (~USD 100–300/month)
- Intensified monitoring and specialist visits
- Complications (neuropathy, retinopathy, nephropathy) requiring advanced care
- Productivity losses and disability
Estimated lifetime healthcare savings: USD 40,000–60,000+ through diabetes prevention.
The Global Health Check Market: Rapid Expansion and Opportunity (2022–2026)
The preventive healthcare and health screening market is experiencing explosive growth, driven by rising chronic disease burden, aging populations, government initiatives, and growing consumer health consciousness.
| Year | Preventive Healthcare Market (Global) | Medical Health Screening Services | Preventive Healthcare Technologies & Services | Key Market Milestones |
| 2022 | USD 243 billion | ~USD 20B (est.) | ~USD 280B (est.) | Post-COVID surge in preventive care awareness; increased telehealth integration |
| 2023 | ~USD 310B (est.) | ~USD 25B (est.) | ~USD 315B (est.) | USPSTF updates recommendations; diagnostic technology advancement; corporate wellness programs expand |
| 2024 | USD 388.17 billion | USD 29.8 billion (600M screenings performed) | USD 300.58 billion | Personalized medicine and AI integration; wearable health tech proliferation; workplace screening mandates increase |
| 2025 | USD 439 billion (projected) | USD 29.56–30B | USD 336–366.91 billion | Screening volume projected to reach 750M; direct-to-consumer testing booms; telehealth + screening hybrid models; genomic screening expansion |
| 2026 (Projected) | USD 480–500B (est.) | USD 32–35B (est.) | USD 380–400B (est.) | AI-powered risk stratification; multi-disease screening bundles become standard; regional/remote screening access expands; insurance reimbursement improves |
Key Market Insights
- Segment Breakdown (2024): Cardiovascular screening dominates at 38% market share, cancer screening at 30%, diabetes screening at 20%, with remaining 12% distributed across other conditions.
- CAGR Acceleration: Preventive healthcare technologies and services are growing at 11.8–14.1% CAGR, substantially outpacing broader healthcare market growth, indicating strong consumer and institutional demand for prevention-focused solutions.
- Regional Growth: Asia-Pacific, particularly India and China, are emerging as high-growth markets. India’s preventive healthcare segment is projected to grow at 9.1% CAGR through 2035, driven by corporate sector expansion and workplace wellness adoption.
- Technology Integration: AI-driven risk stratification, wearable devices synchronized with screening platforms, and direct-to-consumer at-home testing kits are reshaping market dynamics and expanding access beyond traditional clinical settings.
- On-Site/Workplace Preventive Care: A dedicated market segment, projected to grow from USD 26.21 billion (2024) to USD 43.52 billion (2034), reflects corporate investment in employee health as a productivity and retention strategy.
Best Practices for Maximizing the Value of Your Health Check
- Schedule Strategically: Annual checks are ideal for most adults; those with chronic diseases, family history, or multiple risk factors may benefit from semi-annual assessments.
- Prepare Thoroughly: Maintain a list of medications, supplements, and family health history. Fast 8–12 hours before blood draw for accurate lipid and glucose results.
- Communicate Actively: Discuss lifestyle factors (smoking, alcohol, physical activity), mental health concerns, and specific symptom worries with your healthcare provider.
- Follow-Up Promptly: If abnormal results are found, attend recommended follow-up appointments and specialist referrals without delay.
- Implement Recommendations: Early intervention based on screening results—lifestyle modification, medication initiation, or intensified monitoring—determines whether screening translates into actual health improvement.
- Leverage Digital Integration: Use health records portals, wearable devices, and health tracking apps to monitor trends and maintain continuity between visits.
Conclusion
Health checks represent one of modern medicine’s most powerful and cost-effective tools for extending lifespan, improving quality of life, and reducing the staggering global burden of chronic disease. The 45% reduction in all-cause mortality associated with annual preventive assessment, coupled with the documented early detection of life-threatening cancers, the prevention of type 2 diabetes through lifestyle intervention, and dramatic long-term healthcare cost savings, make health checks an investment every individual should prioritize.
With the global preventive healthcare market projected to reach USD 439 billion in 2025 and accelerating growth through 2026, innovative screening technologies, personalized risk assessment, and expanded access through telehealth and workplace programs are making comprehensive health checks more accessible, affordable, and actionable than ever before. Whether you are 25 or 75, gender-specific, age-appropriate health screenings tailored to your risk profile should form the cornerstone of your lifelong wellness strategy.