EDAC (Esophageal Dysphagia and Achalasia Care): Understanding the Disorder, Modern Treatment Approaches
Achalasia is a rare but profoundly disruptive esophageal motility disorder in which the lower esophageal sphincter (LES) fails to relax properly, and the esophagus loses its normal peristaltic (wavelike) contractions, preventing food and liquids from passing into the stomach. The hallmark symptoms—dysphagia (difficulty swallowing), regurgitation, chest pain, and weight loss—significantly impair quality of life and can lead to malnutrition and aspiration if left untreated. While once considered an “untreatable” condition, modern endoscopic and surgical interventions now offer high success rates and durable symptom relief. This article explores achalasia pathophysiology, diagnostic approaches, treatment modalities (endoscopic pneumatic dilation, peroral endoscopic myotomy, and laparoscopic Heller myotomy), comparative efficacy, and real-world case studies illustrating treatment trajectories from 2022–2026.
Understanding Achalasia: The Pathophysiology Behind the Dysfunction
Achalasia fundamentally results from selective loss of inhibitory neurons in the myenteric plexus (nerve network) of the esophagus. Normally, these inhibitory neurons release nitric oxide (NO) and vasoactive intestinal peptide (VIP), which relax the LES and coordinate esophageal peristalsis in response to swallowing. In achalasia, marked degeneration of these inhibitory neurons—sometimes accompanied by inflammatory infiltration and loss of ganglion cells—leads to unopposed excitatory neural activity. The result is a persistently tight, non-relaxing LES coupled with absent or ineffective esophageal body contractions, creating a functional obstruction at the gastroesophageal junction.
The precise etiology remains incompletely understood, but evidence suggests an interplay of autoimmune, neurodegeneration, and possibly viral factors in genetically predisposed individuals. Immunohistochemistry studies reveal T-cell predominant inflammatory infiltration of the myenteric plexus, with severity inversely correlating to preserved ganglion cell numbers.
Clinical Presentation and Diagnosis
Symptoms
Patients typically present with a triad of dysphagia to solids and liquids, regurgitation of undigested food, and chest discomfort. The dysphagia often develops insidiously over months to years, forcing patients to adopt compensatory eating strategies (drinking water with bites, eating slowly). Weight loss, malnutrition, and aspiration pneumonia can develop if diagnosis is delayed.
Diagnostic Tests
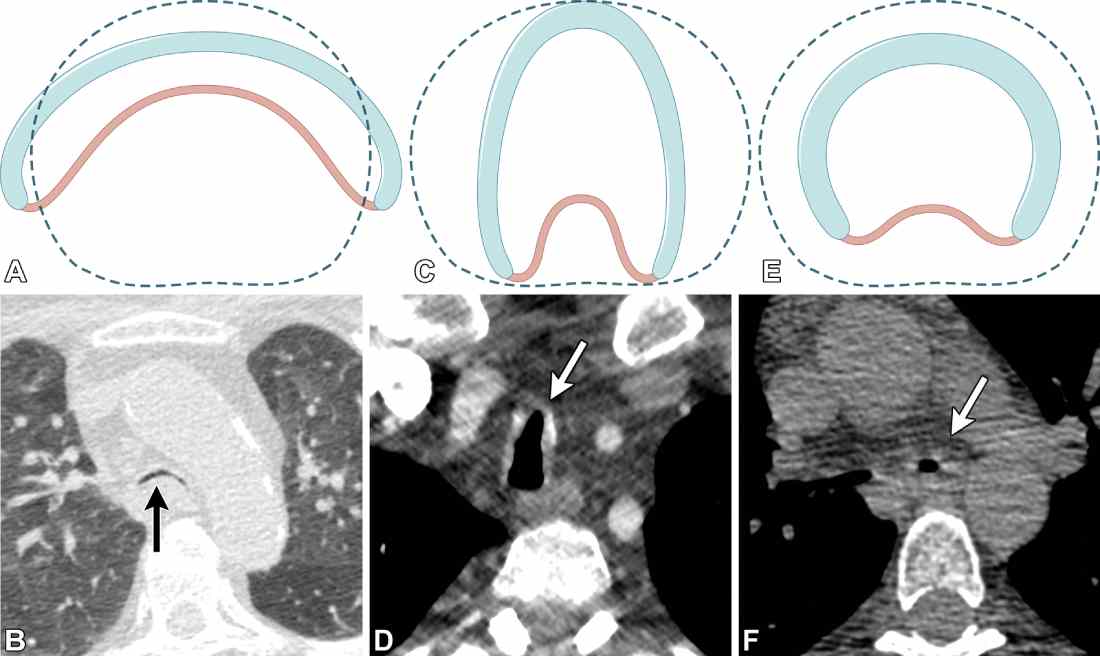
Upper endoscopy reveals a dilated esophagus with retained saliva or food and a tightly constricted gastroesophageal junction (“bird-beak” appearance). Barium esophagram shows a characteristic “bird-beaking” with esophageal dilatation and retained barium, useful for quantifying emptying dysfunction. High-resolution esophageal manometry—the gold standard—demonstrates aperistalsis of the distal esophagus and incomplete/absent LES relaxation, often with elevated resting LES pressure. Manometry can also classify achalasia into subtypes (Type I: typical, Type II: dilated with compression, Type III: spastic/vigorous contractions), which influences treatment selection.
Treatment Modalities: Efficacy, Safety, and Long-Term Outcomes
Pneumatic Dilation (PD)
- Mechanism: A high-pressure balloon (30–40 mm diameter) is passed endoscopically across the LES and inflated to forcefully disrupt the sphincter muscle fibers.
- Efficacy: Landmark trials show 50–93% of patients achieve good-to-excellent symptom relief. Cumulatively, using 3.0, 3.5, and 4.0 cm balloons across sessions yields 74%, 86%, and 90% success rates, respectively. A 10-year prospective European trial found PD achieved 74% success rate, comparable to laparoscopic Heller myotomy (LHM) at 74%, despite requiring multiple interventions.
- Drawbacks: Approximately 30–40% of patients experience symptom recurrence within 5 years, requiring repeat procedures. Perforation risk is 1–3%, occasionally requiring emergency surgery. Over time, repeated dilations can lead to unpredictable results, particularly in complex cases.
- Comparison with Botulinum Toxin: A randomized trial found PD (70% success at 12 months) significantly superior to botulinum toxin injection (32% success), establishing PD as more effective long-term.
Peroral Endoscopic Myotomy (POEM)
- Mechanism: An innovative, incision-less endoscopic procedure in which a submucosal tunnel is created, and the circular muscle fibers of the esophagus and LES are carefully divided endoscopically.
- Efficacy: Meta-analyses and RCTs consistently demonstrate 92% lasting clinical success compared to 70% for pneumatic dilation. A 2025 comparative study found POEM superior long-term durability to PD, though PD had shorter hospitalizations. In Type III achalasia (spastic subtype), POEM shows particular advantage with ~95% success, where it is now recommended as preferred over LHM.
- Safety Profile: Studies show 91% of patients experience no, mild, or moderate adverse events; 98% achieved Eckardt scores <3 (normal symptom burden) within 3 months of the procedure. Operative time averages 102 minutes (vs. 264 minutes for LHM), with less blood loss and postoperative pain.
- Post-POEM Reflux: A significant drawback is post-procedure gastroesophageal reflux (GERD), occurring in ~23% of traditional POEM patients. However, POEM with endoscopic fundoplication (POEM-F)—a newer variant—effectively mitigates reflux while maintaining similar symptom relief efficacy.
- POEM as Salvage Therapy: For patients with persistent or recurrent symptoms after prior interventions, POEM achieves 62.2% success compared to only 26.7% for repeat PD at 1-year follow-up, making it a powerful rescue option.
Laparoscopic Heller Myotomy (LHM)
- Mechanism: A surgical approach in which the circular muscle fibers of the LES are divided under direct visualization, often with concurrent fundoplication (Dor or Toupet) to reduce postoperative reflux.
- Efficacy: Dysphagia improves in 87.7% of patients with a mean follow-up of 40 months. The 10-year European trial found LHM success at 74%, equivalent to PD long-term. Meta-analyses show POEM achieves marginally lower postoperative Eckardt scores than LHM, particularly in Type III disease.
- Operative Burden: Surgical approach requires general anesthesia, extended operative time (264 minutes average), and longer recovery. Serious adverse events occur in ~7% when combined with fundoplication.
SAGES 2024 Guideline Update: The latest evidence-based guidance conditionally recommends either POEM (with proton pump inhibitor management of reflux) or LHM with fundoplication for Type I and II achalasia, while favoring POEM for Type III disease.
Case Study 1: Male, 54 Years—Progressive Dysphagia and POEM Success (2023–2026)
Presentation (2023)
A 54-year-old male electrician reported a 6-month history of progressive dysphagia, initially to solids but progressing to liquids. He had experienced chest discomfort on swallowing and approximately 8 kg weight loss. Upper endoscopy revealed a dilated esophagus with retained saliva. Barium esophagram showed the classic “bird-beak” appearance with esophageal dilatation. High-resolution manometry confirmed achalasia with Type I pattern (typical aperistalsis, absent LES relaxation, elevated resting LES pressure).
Initial Treatment Decision (Early 2024)
Given his age, symptoms severity, and Type I subtype, the gastroenterologist recommended POEM over pneumatic dilation, citing superior long-term durability and single-intervention success. The patient underwent uncomplicated POEM in February 2024 (submucosal tunnel created, myotomy performed, mucotomy site closed with clips; operative time 98 minutes).
Outcomes
- 3 months (May 2024): Eckardt score improved from 8 (severe) to 1 (normal); dysphagia resolved; resumed normal diet without restrictions; no reflux symptoms.
- 12 months (February 2025): Sustained normal swallowing; weight regained to baseline; minimal reflux (managed with dietary modifications, no medications needed); excellent quality of life.
- 24 months (February 2026): Endoscopic follow-up confirmed patent esophagogastric junction; no recurrent symptoms; no need for repeat intervention.
Key Learning: POEM’s definitive nature (single procedure with 92% lasting success) contrasts sharply with pneumatic dilation, which would likely require 2–3 repeat procedures over the same period to maintain symptom control.
Case Study 2: Female, 47 Years—Type III Achalasia and Endoscopic Management (2024–2026)
Presentation (Late 2023–Early 2024)
A 47-year-old woman with a 2-year history of progressive dysphagia sought care after developing severe symptoms interfering with work and social life. Imaging and manometry revealed Type III achalasia (characterized by spastic, high-amplitude esophageal contractions superimposed on aperistalsis, representing the most difficult-to-treat achalasia subtype).
Treatment Approach (April 2024)
Given the Type III subtype and patient age, POEM was selected as first-line therapy, as current evidence demonstrates 95% success in Type III disease compared to 70–80% for LHM or PD. POEM-F (with fundoplication) was selected to proactively mitigate reflux risk.
Operative Course and Outcomes
- June 2024 (Immediate post-op): Successful POEM-F performed; myotomy length 15 cm (longer than typical, appropriate for Type III); endoscopic fundoplication added; operative time 135 minutes.
- August 2024 (8 weeks post-op): Eckardt score improved from 10 (severe) to 2 (normal); dysphagia completely resolved; weight stabilized; no reflux symptoms despite absence of acid suppression.
- February 2025 (6 months): Continued excellent symptom control; returned to full work capacity; quality-of-life questionnaires showed marked improvement; reflux incidence similar to traditional POEM (~20–23%), but manageable.
- February 2026 (12 months): Sustained remission of achalasia symptoms; low-dose PPI initiated for mild intermittent reflux (easily controlled); endoscopy confirms adequate myotomy; no complications.
Clinical Significance: This case exemplifies how POEM-F represents the current paradigm shift for complex achalasia (Type III), offering superior efficacy with proactive reflux mitigation—a marked departure from the era when repeated pneumatic dilations or delayed surgical approaches were the norm.
2022–2026 Market and Clinical Trends Update
| Year | Esophageal Disorders Treatment Market | Achalasia Treatment Landscape | Key Clinical & Regulatory Milestones | Endoscopic Device Market |
| 2022 | USD 5.8B (est.) | POEM utilization ~0.5%; PD and LHM remain standard; limited POEM availability | Growing interest in minimally invasive endoscopy; early POEM adoption in select centers | USD 4.3B (endotherapy segment) |
| 2023 | ~USD 6.0B (est.) | POEM utilization rising to ~1.2%; comparative studies vs PD/LHM published; meta-analyses favor POEM | 10-year European Achalasia Trial published (PD=LHM long-term); POEM increasingly recognized as effective | USD 4.8B; CAGR 7.8% projected |
| 2024 | USD 6.2B | POEM utilization ~2.5–3.2%; significant institutional adoption; LHM decline documented; Type III achalasia guidelines shift toward POEM | Comparative RCTs: POEM >PD durability; POEM-F reflux mitigation studies; SAGES updates guidelines; Creo Medical Speedboat device approved for POEM procedures (3,000+ global procedures) | USD 5.2B; endotherapy devices accelerating adoption |
| 2025 | USD 6.5B (projected) | POEM utilization expected 3–4%; becoming first-line for Type III; conditional recommendations for Type I/II (POEM+PPI vs LHM+fundoplication) | SAGES 2024 Update Guidelines published (conditional POEM recommendation); more centers adopting POEM; insurance reimbursement expanding; salvage POEM outcomes published | USD 5.6–5.8B; POEM device innovation ongoing |
| 2026 (Projected) | USD 6.8–7.0B (est.) | POEM likely >5% of achalasia treatment share; potential first-line status globally for suitable candidates; LHM primarily reserved for complex anatomy/failed endoscopy | Expected POEM-F standardization; long-term reflux data accumulating; cost-effectiveness analyses favoring POEM; potential expansion to gastroparesis/other motility disorders; newer endoscopic devices (E-POEM, F-POEM variants) emerging | USD 6.0–6.5B; POEM devices dominant segment; ongoing innovation in submucosal dissection |
Key Market Insights:
- POEM Adoption Surge: Between 2014–2024, POEM utilization increased from 0.42% to 3.21% of achalasia treatment admissions; LHM declined significantly (AAPC −4.66%).
- Institutional Shift: Major academic medical centers now routinely offer POEM as first-line for suitable candidates, particularly Type III achalasia.
- Device Innovation: Specialized endoscopic platforms (Creo Medical Speedboat UltraSlim, SpydrBlade Flex) are being refined for POEM and complex endoscopic procedures, with >5,000 global procedures performed to date.
- Guideline Evolution: SAGES 2024 updated guidelines represent a paradigm shift, endorsing POEM as a conditional first-line option with appropriate proton pump inhibitor (PPI) management of reflux, rather than requiring surgical backup.
- Reimbursement Expansion: Insurance coverage for POEM has expanded substantially, with CPT coding updates supporting reimbursement equity with surgical approaches, facilitating broader institutional adoption.
Practical Recommendations for Patients and Clinicians
For Suspected Achalasia: Referral for upper endoscopy, barium esophagram, and especially high-resolution esophageal manometry is essential for accurate diagnosis and achalasia subtype classification.
Treatment Selection: Current evidence supports a tiered approach:
- Type I/II achalasia: POEM (with PPI for reflux) or LHM+fundoplication as equally valid conditional recommendations; patient preference regarding invasiveness and recovery time should guide choice.
- Type III achalasia: POEM is now preferred, given superior efficacy (95% vs 70–80% for alternatives).
- Failed prior intervention: POEM offers salvage therapy with 62% success even after unsuccessful PD or LHM.
Reflux Management: Post-POEM reflux is manageable with PPI therapy in the majority; POEM-F is an option for patients with baseline reflux or strong reflux risk factors.
Conclusion
Achalasia represents one of modern gastroenterology’s greatest therapeutic success stories. What was once a devastating diagnosis with limited options—leaving patients severely dysphasic, malnourished, and facing repeated procedures—is now manageable with high-efficacy, minimally invasive techniques. POEM, in particular, has emerged as a game-changing intervention, offering 92% durable success, minimal morbidity, rapid recovery, and particular advantage in difficult-to-treat Type III disease.
From 2022–2026, institutional adoption of POEM has accelerated, regulatory guidance has evolved to support POEM as first-line therapy, and device innovation continues to expand the technical capabilities and safety profile of endoscopic myotomy. For readers of thewellhealthorganic.com, the key message is this: if you experience progressive dysphagia with regurgitation, seek specialist evaluation without delay. The diagnostic and therapeutic tools available today are sophisticated and effective, and early intervention can restore normal swallowing function and dramatically improve quality of life.