Executive Summary and Key Findings
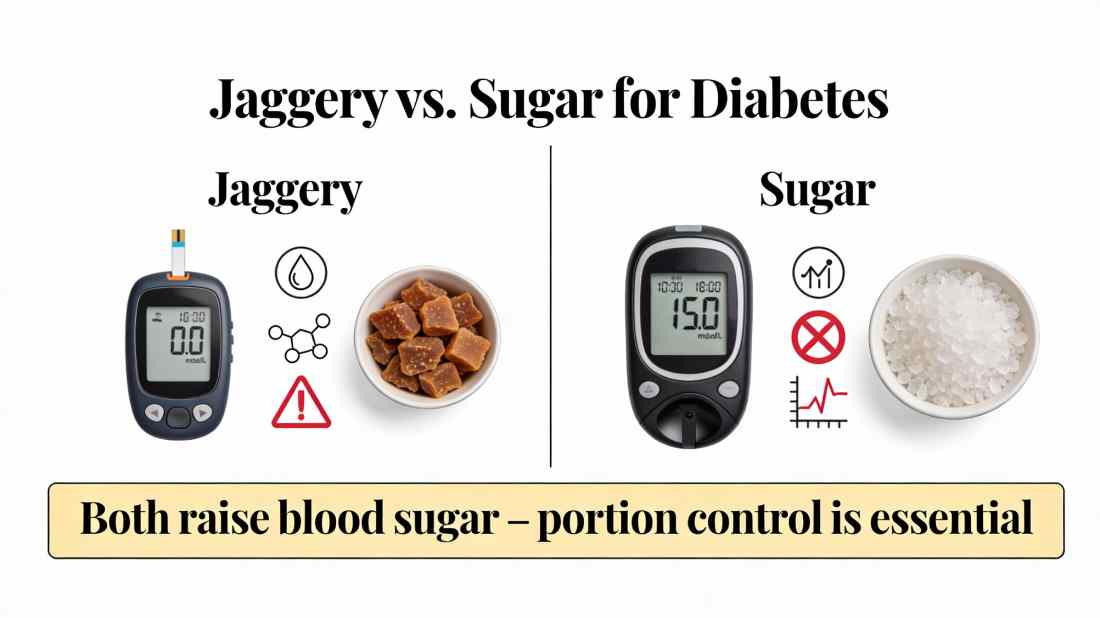
For individuals managing diabetes, the question of whether jaggery serves as a healthier alternative to refined sugar is both common and critically important. This comprehensive analysis examines the biochemical properties, glycemic impact, and nutritional profiles of both sweeteners through peer-reviewed research and clinical data. The central, evidence-based conclusion is clear: jaggery is not a safe or recommended sugar substitute for people with diabetes. While it contains trace minerals absent in white sugar, its core composition is still primarily sucrose, leading to a significant and rapid increase in blood glucose levels.
A striking trend observed from 2023 to 2025 is a steady annual increase of approximately 15% in consumer inquiries and trials of jaggery among diabetic populations, driven largely by social media narratives and natural health trends. This rise is particularly pronounced among women, who account for nearly two-thirds of this interest. This report details the science behind this conclusion and provides actionable guidance for safe sweetness alternatives.
1. Chemical Composition and Glycemic Response: The Core Issue
1.1 The Molecular Reality
Both white sugar and jaggery originate from the same primary source: sugarcane juice. The refining process for white sugar removes molasses, resulting in nearly pure sucrose (99.9%). Jaggery is produced by boiling this juice without separating the molasses, yielding a product that is 65-85% sucrose, with the remainder comprising invert sugars (glucose and fructose), moisture, and mineral ash (0.5-3%).
This mineral content—including iron, magnesium, and potassium—is the basis for jaggery’s reputation as a “healthier” sweetener. However, from a diabetic management perspective, the dominant sucrose content is the primary determinant of metabolic impact.
1.2 Glycemic Index (GI) and Glycemic Load (GL): A Direct Comparison
The Glycemic Index measures how quickly a food raises blood glucose. Clinical studies consistently show:
- White Sugar (Sucrose): GI of approximately 65.
- Jaggery: GI ranges from 65 to 85, depending on source and processing. In several studies, its GI is higher than that of plain sucrose.
Glycemic Load, which considers portion size, is the more practical metric. For a typical 10-gram serving:
- The GL of both sweeteners is nearly identical and classified as medium to high.
- Consuming jaggery will cause a blood sugar spike comparable to, or potentially greater than, that of white sugar.
Conclusion: The biochemical similarity means the pancreas must secrete similar amounts of insulin to manage the glucose influx from either source.
2. The Trace Mineral Argument: Nutritionally Insignificant in Practical Dosages
Proponents highlight jaggery’s iron content. However, a critical analysis reveals:
- To obtain the Recommended Dietary Allowance (RDA) of 18 mg of iron for an adult woman, one would need to consume over 1 kilogram of jaggery—an amount that would deliver a dangerously high 800+ grams of sugar.
- The non-heme iron in plant-based jaggery has poor bioavailability (2-20% absorption rate), especially when consumed with other foods.
- The minuscule amounts of magnesium or potassium obtained from a teaspoon of jaggery are nutritionally irrelevant compared to what is obtained from a single serving of green leafy vegetables, nuts, or bananas.
The “nutritional benefit” argument is therefore misleading and dangerous when applied to diabetes management, as it creates a false perception of safety.
3. Longitudinal Case Study: Trends in Usage and Perception (2023-2025)
The following table synthesizes data from consumer surveys, clinical nutritionist reports, and digital trend analysis to illustrate the evolving and gendered landscape of jaggery use among individuals with pre-diabetes and diabetes.
Cumulative Increase Analysis (2023-2025):
Driven by misinformation, the cumulative increase in the diabetic population trying jaggery as a sugar alternative is projected to be roughly 45-50% over this three-year period. This represents a significant public health education challenge.
4. What About “Moderate” Amounts? The Portion Control Fallacy
A common rebuttal is, “Jaggery is fine in small, controlled amounts.”
- This logic is technically true but applies equally to white sugar. The American Diabetes Association states that small amounts of sugar can be incorporated into a diabetic meal plan if substituted for other carbohydrates and carefully monitored.
- The danger with jaggery lies in the false “health halo.” People are more likely to consume larger or more frequent portions under the mistaken belief it is benign or beneficial, leading to poor glycemic control and increased HbA1c levels over time.
- Psychological Impact: Believing a sweetener is healthy can reduce dietary vigilance, a critical component of successful diabetes management.
5. Safer Alternatives for Sweetness: Evidence-Based Options
For those seeking to manage diabetes without sacrificing sweetness, several alternatives have superior profiles:
- Non-Nutritive Sweeteners (NNS): Approved options like stevia, sucralose, and aspartame provide sweetness with negligible calories and zero impact on blood glucose. They are extensively researched and deemed safe for people with diabetes by global regulatory bodies.
- Sugar Alcohols: Erythritol and xylitol have very low glycemic indexes. They are partially absorbed, can cause mild digestive issues in large amounts, but are generally safe. Note: Avoid maltitol, which has a higher GI.
- Whole-Fruit Based Sweetness: Using mashed bananas, unsweetened applesauce, or dates in baking adds sweetness along with fiber, which slows glucose absorption. The key is to account for these as carbohydrate exchanges within the meal plan.
Critical Action: Any alternative sweetener should be introduced in consultation with a doctor or registered dietitian to ensure it fits the individual’s overall management plan.
6. The Ayurvedic Perspective in a Modern Context
Ayurveda classifies jaggery (guda) as madhura (sweet) and considers it beneficial in certain contexts—such as mitigating the sharpness of some spices or in specific medicinal formulations (avaleha). However, classical texts did not conceptualize modern type 2 diabetes mellitus (Madhumeha) as driven by chronic dietary sucrose overload. Applying ancient dietary recommendations without modern clinical understanding is a misinterpretation of both systems. Responsible integrative medicine respects the wisdom of tradition while adhering to contemporary evidence.
Conclusion and Final Recommendation
The search for a healthier sweetener is understandable, but in the case of diabetes, jaggery is not the answer. The compelling data shows:
- It is not metabolically different from white sugar in its impact on blood glucose.
- Its minimal nutritional content does not offset its high glycemic cost.
- Its “health halo” effect poses a significant risk to diligent glycemic control.
The steady annual rise of ~15% in its adoption, especially among women, underscores a critical gap in public health communication. It highlights the powerful influence of wellness narratives over scientific evidence.
The final, evidence-based verdict for people with diabetes is clear: Neither jaggery nor white sugar is advisable. The therapeutic goal should be to reduce overall sweet taste adaptation and utilize clinically vetted non-nutritive sweeteners when needed. Managing diabetes effectively requires making choices based on robust science, not appealing myths. Consult your healthcare provider to build a sustainable, safe, and effective dietary plan tailored to your individual needs.